PANCREATIC DUCT
There is a a main pancreatic duct and an accessory pancreatic duct. The main pancreatic duct (MPD) drains the the tail, body and the ventral portion of the head. The accessory duct has variable connection to the MPD, and the secondary papilla in the duodenum.
The main pancreatic duct joins with the common bile duct to form the ampulla, which opens into the duodenum. This configuration occurs in 90% of people.
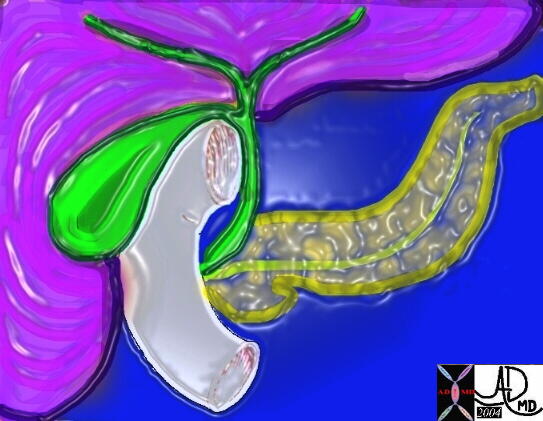
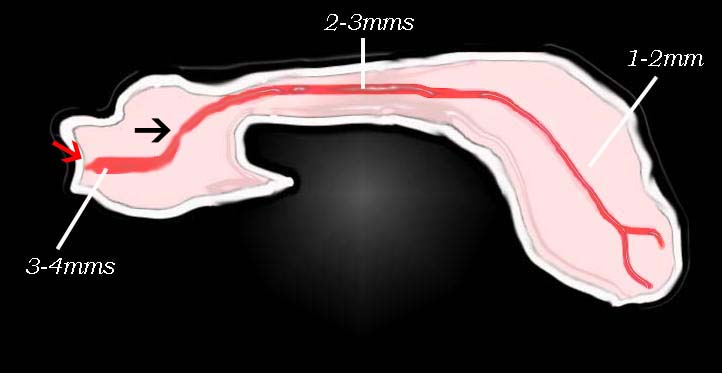
In this image the MPD is shown joining the CBD at the doudenum. Courtesy Ashley Davidoff 22391 R W3
The minor pancreatic duct usually enters independantly into the duodenum 2cms cranial to the major papilla. An accessory pancreatic duct (persistent duct of Santorini) that drains into the minor ampulla is present in 44% of individuals. The duct of Santorini provides the major drainage route in 9% of people.
MAIN PANCREATIC DUCT
The main pancreatic duct is composed of the dorsal duct of the tail and body which has joined the ventral components of the duct that drains the head and uncinate process. The pancreatic duct receives 20–35 short tributaries that enter at right angles. Interlobular ducts are found between lobules, within the connective tissue septae. They vary considerably in size. The smaller forms have a cuboidal epithelium, and the larger interlobular secondary ducts are lined by columnar columnar epithelium . Intralobular ducts transmit secretions into the interlobular ducts.
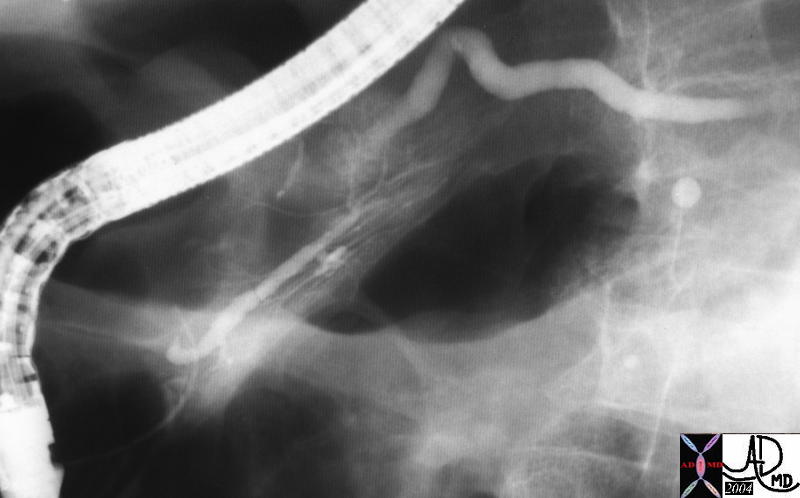
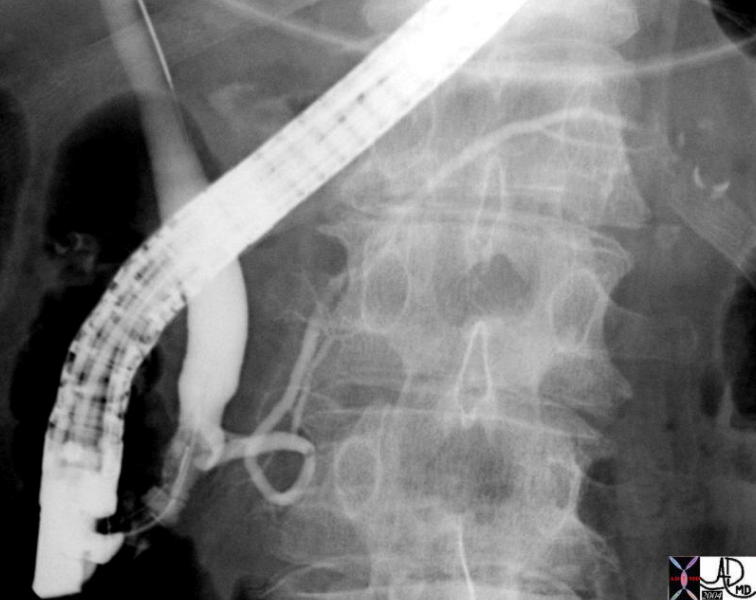
This ERCP shows the claasic confluence of the MPD with the CBD. The slight tortuosity of the MPD by the neck of the pancreas is a normal variant. Neither the accessory duct nor the secondary branches is seen. Parts of the cystic duct and gallbladder are seen in the RUQ. 29247 Courtesy Ashley Davidoff MD
Size of the Pancreatic Duct
The length of the MPD varies between 10 and 20 cms, which is quite a wide variation in size. The length of the duct has no functional nor anatomic significance.
The normal internal dimensions of the tail range from 1.5mm to 3mms; the body 2.5-5mms and the head 3.5- 6.5mms (Sivak)
A duct that is 6.5mms in diameter can appear quite dilated. In the setting of an ERCP if such a “large” duct is encounteresd in the head of the pancreas a drainage film after 5 minutes should be obtained. The normal duct will empty by this time and a dilated duct will contain retained contrast at 10 minutes.
The normal duct size that is quoted depends on the modality being used to measure. Since at ERCP contrast is injected, there is an overestimate of the true size.
The average maximum diameter of the main pancreatic duct (autopsy series), was 2.9 mm (<50yrs) and 3.5 mm (>50years).
On ERCP the duct is 3 to 4 mm in the head, 2 to 3 mm in the body, and 1 to 2 mm in the tail.
The upper limits of a normal duct diameter on CT is considered to be 2 to 3 mm in the body and tail, and up to 5 mm in the head.
The length of the pancreatic duct is variable; however, mean length is approximately 205 mm, with a range of 107 to 270 mm.
Normal intrapancreatic structures on US include the common bile duct, pancreatic duct, and some small arterial and venous branches. The intrapancreatic common bile duct measures up to 4 mm in internal diameter. The MPD of of Wirsung can be seen in the body of the pancreas in about 80% of patients, either as a tube or as an echogenic line. The normal diameter ranges between .8mm to 3 mm. The duct is usually slightly larger in the head.
The generally accepted size of the pancreatic duct using US is less than 2mm, and up to 3mms in the head. The size does increase with age and the duct dilates in patients with gallstones. In acute pancreatitis the duct also enlarges up to 3mm and regresses in size as the patient improves. However it may not return to normal following the episode.
Although the duct enlarges with age, but the duct in the body should not exceed 3mm. (Glaser)
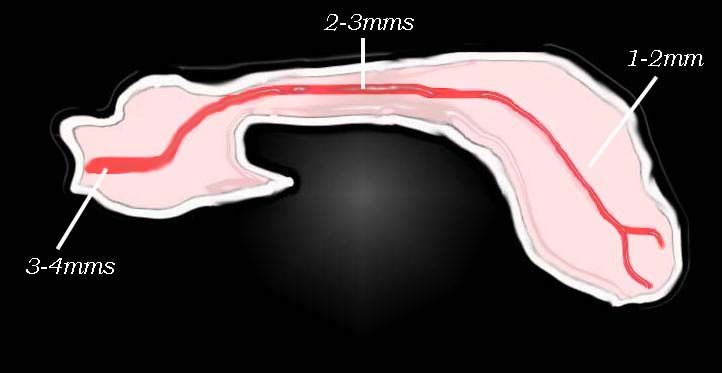
This diagram shows the normal values of the pancreatic duct in the head body and tail.
Courtesy Ashley Davidoff MD. 41394size002b02L
Size of the The Ampulla
varies in width from 1.5mms to 4.5mms and its lenth varies from 1-14mms
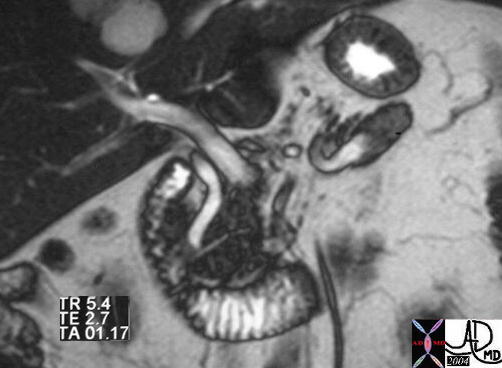
The dynamic MRI with gadolinium shows a prominent but normal main pancreatic duct. The duct is sometimes positioned in the middle of the gland (as in ths case), but it can be both anteriorly and posteriorly positioned. The distal MPD is seen nearing the larger distal CBD. 19955 Courtesy Ashley Davidoff MD
The confluence of the CBD and MPD are seen in the head of the pancreas in this MRCP which also demonstrates the intimate relationship of the head of the pancreas with the C-sweep of the duodenum. 28070b Courtesy Ashley Davidoff MD
The normal pancreatic duct can usually be visualised on an MRCP. In this case the MPD of the neck, body and tail are demonstrated. 39958 Courtesy Ashley Davidoff MD
The Accessory Duct of Santorini
The accessory duct of Santorini (APD) is a remnant of the former main pancreatic duct that was a continuum of the duct in the neck body and tail with the dorsal portion of the duct. With the rotation of the ventral portion from the lateral aspoect of the duodenum to the medial side, the duct of the body and tail lose their connection with the dorsal portion of the head and form a bond with the ventral duct, isolating the dorsal duct. he result of how the dorsal duct ends up is very variable and except for pancreas divisum usually has no significant consequence. he duct may be blind, keep some connection with the main duct, retain a full embryologic connection with the duct of the body divisum or drain independantly into the duodenum.
The ERCP demonstrates a smaller accessory duct of Santorini which is filling from the MPD (duct of Wirsung) injection. The accessory duct enters the duodenum more superiorly. 04184 Courtesy Ashley Davidoff MD pancreas pancreatic duct anatomy duct of Wirsung fx dilated dilitation enlarged accessory duct of Santorini ERCP
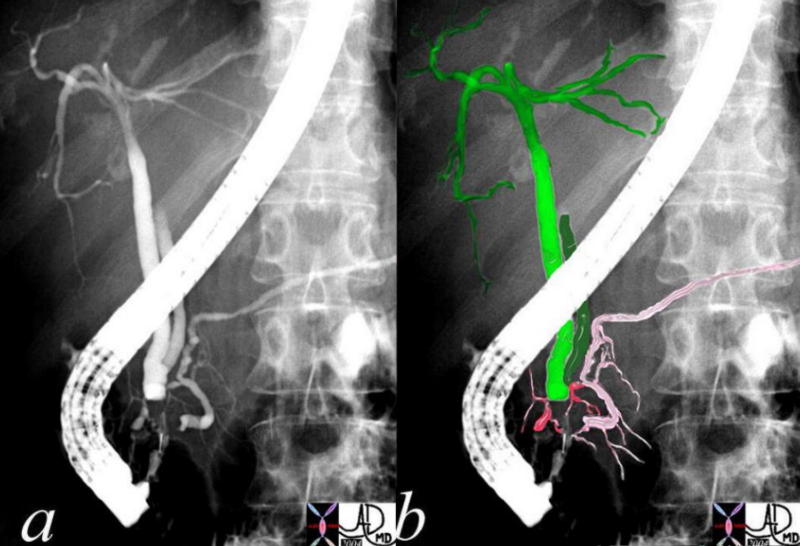
These images from an ERCP shows the CBD, (green) MPD (light pink) and the accessory pancreatic duct (rose). In this instance the MPD and the accessory duct are connected and they both have egress into the duodenum. The secondary ducts in the head are filled, but are not seen in the body or tail. Note also the low lying insertion of the cystic duct(dark green) which is an important anomaly to note for the surgeon.39963c01 Courtesy Ashley Davidoff MD
Shape of the Pancreatic Duct
In general the MPD is “S” shaped and may have some normal narrowings in the expected location where the dorsal and ventral componenets of the ducts fuse. The preampullary region may become fusiform in shape and mildly dilated. There is sometimes a normal loop to the duct in the head of the pancreas.
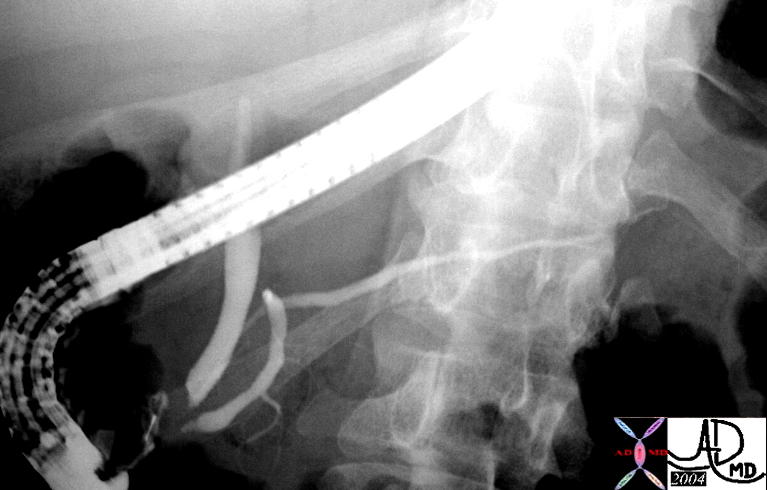
This normal ERCP shows a normal “S” shape to the pancreatic duct. 39962 Courtesy Ashley Davidoff MD code pancreas 39k pancreatic duct normal ampulla imaging radiology ERCP distal CBD
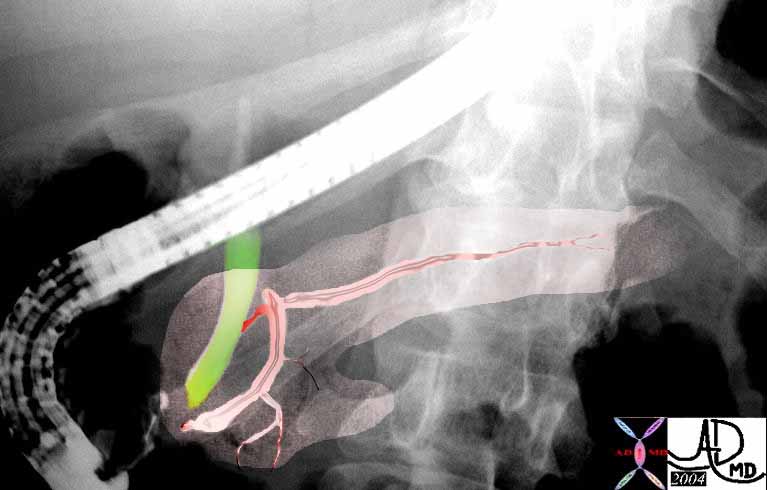
This ERCP is the overlay of the case above it, and it shows the relative positioning of the duct in relation to the pancreas and the bile duct. Note also the 04bifid appearance to the duct in the tail which is a normal and common variant. Courtsy Ashley DAvidoff MD. 39962b04
When the main duct is joined by the parts of the duct in the head and uncinate process, it becomes Y-shaped.
Within the head, the main pancreatic duct turns inferiorly and comes into close relationship with the bile duct. Usually, these two ducts unite to form the hepatopancreatic ampulla (of Vater). The ampulla opens via a common duct into the duodenum at the summit of the major duodenal papilla. The sphincter around the terminal part of the main pancreatic duct is known as the sphincter of the pancreatic duct.
The sphincter around the hepatopancreatic ampulla is called the hepatopancreatic sphincter (of Oddi), which controls both the flow of pancreatic juices and bile.
The tail usually has a bifid pattern and it may fan out into three or more branches.
The pancreatic duct shape and course varies greatly. The most common shape seen in 50% of cases is a descending duct that courses gradually from the superior aspects in the tail to the region of the ampulla. Other variations include sigmoid, vertical, and loop configurations.
When the main duct is joined by the parts of the duct in the head and uncinate process, it becomes Y-shaped. This begins in the tail of the pancreas and runs through the substance of the gland, receiving tributaries in a herringbone pattern.
There are normal narrowings to the duct. The first and most obvious is at the ampulla where the duct narrows as as the sphincter of the pancreatic duct just before it joins the bile duct. The second is not as common but is important to recognise as a variant. It occurs at the junction of the dorsal and ventral ducts in the head of the pancreas. When the narrowing is a normal variant there will be no upstream dilatation and the postdrainage study will show clearing of the contrast from the system.
There are normal narrowings to the duct. The first and most obvious is at the ampulla where the duct narrows as the sphincter of the the pancreatic duct just before it joins the bile duct. The second is not as common but is important to recognise as a variant. It occurs at the junction of the dorsal and ventral ducts in the head of the pancreas 41394size002b04L Courtesy Ashley Davidoff MD
When the main duct is joined by the parts of the duct in the head and uncinate process, it becomes Y-shaped. Within the head, the main pancreatic duct turns inferiorly and comes into close relationship with the bile duct.
Usually, these two ducts unite to form the hepatopancreatic ampulla (of Vater). The ampulla opens via a common duct into the duodenum at the summit of the major duodenal papilla.
The sphincter around the terminal part of the main pancreatic duct is known as the sphincter of the pancreatic duct.
The sphincter around the hepatopancreatic ampulla is called the hepatopancreatic sphincter (of Oddi), which controls both the flow of pancreatic juices and bile.
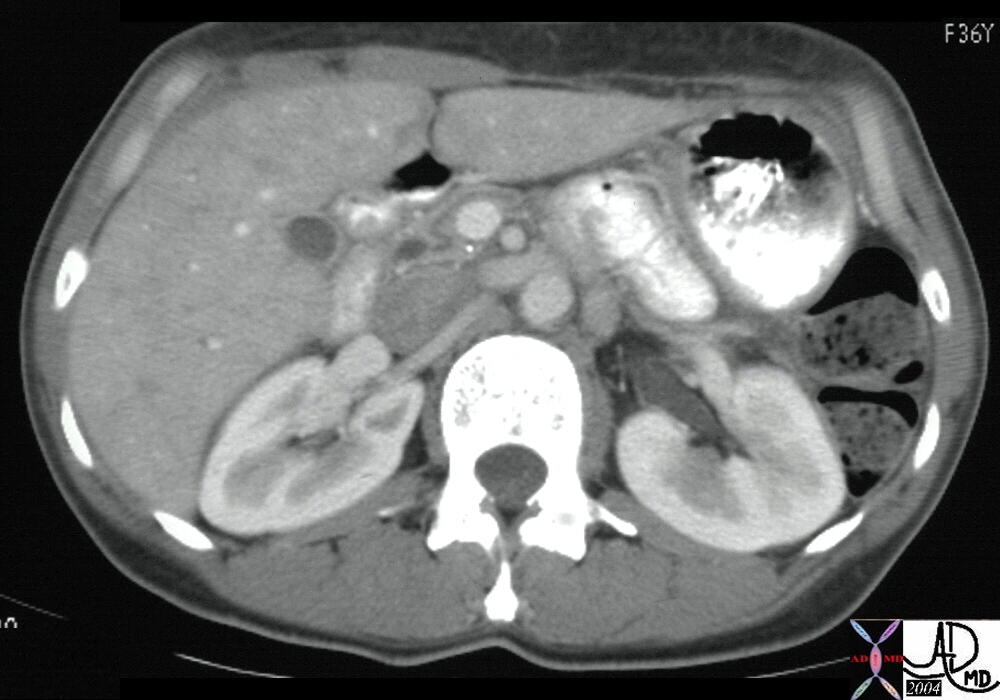
The CT of the abdomen from a 36year old female shows a relative atrophy of the head of the pancreas with secondary prominence of the MPD. The size and shape of the duct are normal. The curved appearance of the duct in the head is a normal variant. The pancreatic at this stage is separate but very close to the larger distal CBD. 25182 Courtesy Ashley Davidoff MD
A normal loop of the MPD in the head of the pancreas. In this case there does seem to be a filling defect at the 2 oclock position of the loop which seems to have a small tail. It may represent some mucoid materaial. The MPD has a ascending course from the neck to the tail which is the most common variant and occurs in about 50% of cases. 41389 Courtesy Ashley Davidoff MD
An acute bend of the MPD in the neck of the pancreas is also a normal variant. Sometimes the shape of the pancreas and the duct relate to the shape of the body. Since the pancreas is relatively soft and has no capsule its shape can be moulded. The MPD has a descending course from the neck to the tail which only occurs in about 5% of cases.Courtesy Ashley Davidoff MD 41409c02
The course of the main pancreatic duct from the tail to the neck is ascending in about 50% of cases, horizontal in about 35%, sigmoid in about 10%, and descending in about 5%.
Postion of the Pancreatic Duct
The pancreatic duct is situated slightly more poisterior in the gland than aterior.
The main pancreatic duct of Wirsung extends from the tail of the pancreas to the major duodenal papilla or ampulla of Vater (Fig. 93-6 and Fig. 93-7). The average diameter of the duct in the adult tapers from 4 to 2 mm, and it is widest in the head of the gland.14 The main duct is close and almost parallel to the distal common bile duct for 2 to 3 mm before combining to form a common duct channel before opening into the duodenum.
Duct of Santorini
The duct of Santorini represents the remnant of the dorsal ductal supply to the head and it persists in a variety of patterns. Its persistent connection to the duodenum via the minor papilla is seen in 50-70% of patients. When it is not connected to the duodenum it serves as an accessory branch connected to the main ductal system.The accessory pancreatic duct of Santorini, usually communicates with the main duct and passes transversely to the right in the upper part of the head of the pancreas. The duct of Santorini lies anterior to the intrapancreatic common bile duct and usually opens into the proximal portion of the second part of the duodenum at the minor papilla, proximal to the ampulla of Vater. In 2-6% of healthy people pancreas divisum exists. In this anomaly the dorsal duct of the body retains it embryonic union with the dorsal duct in the head and opens separately into the minor duct papilla 1-2 cms upstream of the main papilla. The ventral duct remains rudimentary and opens seprate to or with the CBD.
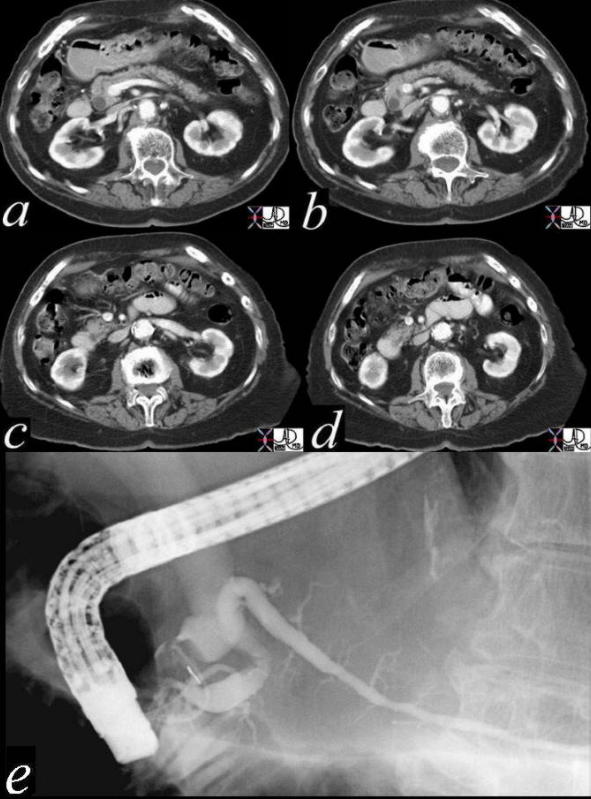
This a case of pancreas divisum as seen by ERCP. The MPD is continuous with the APD of Santorini as it enters the duodenum 1-2cms cranial to the papilla and the entrance of the CBD. 40615 Courtesy Ashley Davidoff MD
This is the injection of the MPD of the case above showing a small ventral duct of Wirsung. The case represents pancreas divisum as seen by ERCP. The main duct was found opening separately within the pailla near the opening of the CBD. 40617 Courtesy Ashley Davidoff MD
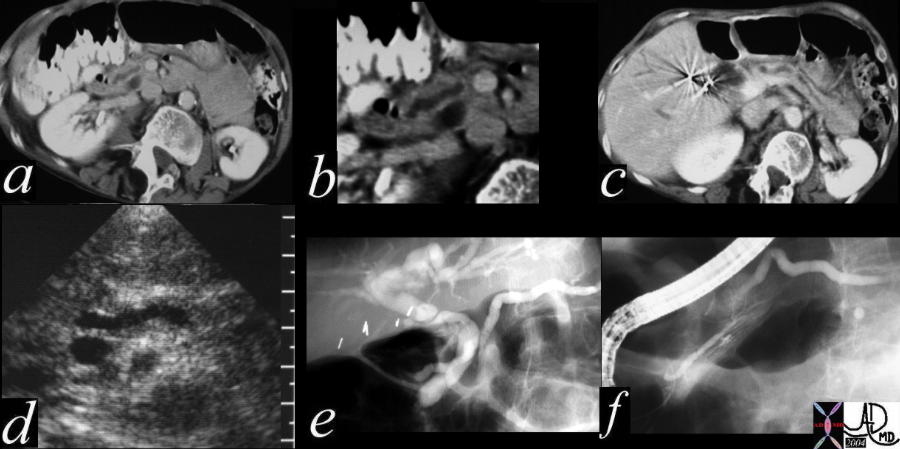
This combination study of pancreas divisum consists of a CTscan with the MPD by passing the CBD (a) magnified in b, with a slightly dilated appearance in the body of the pancreas in c. The US equivalence of this finding is noted in d, while e shows the MPD and ventral duct exiting cranila to the entrance of the CBD. The last injection of the ERCP is the injection of the MPD showing a small ventral duct of Wirsung. The findings are pathognomonic of pancreas divisum. Courtesy Ashley Davidoff MD 40617 c01
Sphinter of Oddi
The sphincter of Oddi consists of circular smooth muscle that surrounds the common channel of the common bile duct and the main pancreatic duct at the ampulla of Vater. The muscle fibers of the sphincter of Oddi extend around the common bile duct just distal to the latter’s oblique entry into the wall of the duodenum to form the choledochal sphincter. A short region of circular smooth muscle also surrounds the pancreatic duct just before its termination to form the pancreatic duct sphincter.
Secondary Side Branches
There are a few generally accepted normal morphologic features of the secondary branches. They are too small to measure but the downstream portions are larger than the upstream branches. In general the side branches in the body and tail arise at approximately 90degrees to the axis of the MPD and have fairly uniform spacing between each branch.

In this ERCP the MPD is dilated and the secondary branches fill and are themselves distended. There are between 25-30 side branches and they come off at right angles to the duct. Courtesy Ashley Davidoff MD 05008
The side branches of the head and uncinate are more varied in their shape. The secondary ductal system may take the form of a dominant single branch with tree like branching or multiple similarly sized branches that fan out.form of the duct
Imaging of the Abnormal Duct
It is extremely important to know and recognise the normal size, shape, position and character of a structure. When there is morphological change due to disease these are the aspects that will change. There are specific section in the “findings of disease” in the mainmenu that adresses the double duct sign, and the dilated duct. Changes of the ducts in diease can also be found in the diseases section. diseases that addresses the are the most common aspects the evaluation of all structure and the pancreatic duct under discussion, that size shape and The changes in chronic pancreatitis include contour irregularities , and dilatation of the main pancreatic duct as well as dilatation of the side branches. The side ranches are not normally seen on MRCP and thus if they are visualised they are dilated.
In severe cases, there is marked dilatation of the side branches resulting in the “chain of lakes” appearance.
Other findings in chronic pancreatitis include stricture formation and intraductal calculi.
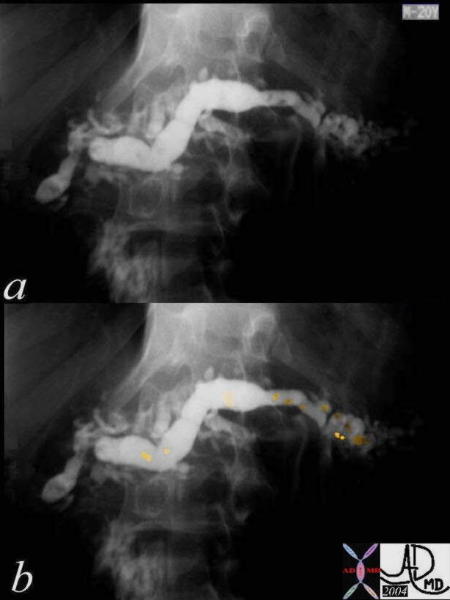
20 year old male with chronic pancreatitis and filling defects on ERCP 40046c Courtesy Ashley Davidoff MD