|
The Common Vein Copyright 2007
Ashley Davidoff MD
Overview
This tumor is a slow growing papillary tumor that arises from the larger ducts and is characterized by the production of abundant mucus. It is usually a benign lesion but has a premalignant predisposition. It occurs more commonly in men in their 7th decade and thus occur in a slightly older group than the mucinous cystadenomas, but the same age group as the serous cystadenomas. Unlike the other mucinous tumors and serous tumors it has a greater predilection for men.
Imaging
The lesion usually occurs in the head of the pancreas, and is associated with a dilated duct. It is suspected when the profuse mucus secretion is noted by the endoscopist.
 This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity in the head of the pancreas. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla. The findings are consistent with the diagnosis of IPMT.18143 Courtesy Ashley Davidoff MD This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity in the head of the pancreas. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla. The findings are consistent with the diagnosis of IPMT.18143 Courtesy Ashley Davidoff MD
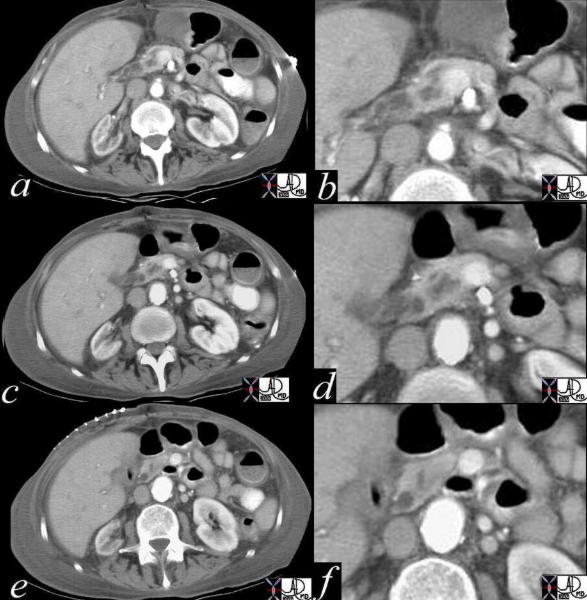 This series of images are from a CT scan of the abdomen taken through the head of the pancreas. Images a,c,and e are magnified in b,d,and f. A heterogeneous and enlarged duct is (a,b,c,d) while the downstream normal appearing duct is seen just before it joins with the bile duct. (e,f) . 18144c01 Courtesy Ashley Davidoff MD This series of images are from a CT scan of the abdomen taken through the head of the pancreas. Images a,c,and e are magnified in b,d,and f. A heterogeneous and enlarged duct is (a,b,c,d) while the downstream normal appearing duct is seen just before it joins with the bile duct. (e,f) . 18144c01 Courtesy Ashley Davidoff MD
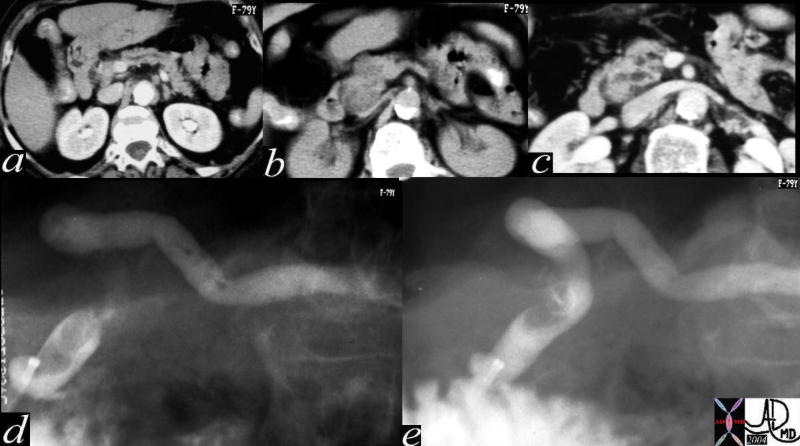 This first series of images are from a CT scan of the abdomen taken through the body and head of the pancreas. A minimally dilated pancreatic duct is noted in the body and neck (a), a heterogeneous mass in the head (b), and a dilated duct in the head and uncinate process(c). Images of the dilated duct with stranding mucoid material and a mass in the distal duct are noted on the ERCP. Mucus was seen emanating from the papilla at ERCP. A diagnosis of mucinous duct ectasia (IPMT) was made. A papillary mucus secreting adenoma was found at surgery consistent with the clinical diagnosis. 40378c Courtesy Ashley Davidoff MD This first series of images are from a CT scan of the abdomen taken through the body and head of the pancreas. A minimally dilated pancreatic duct is noted in the body and neck (a), a heterogeneous mass in the head (b), and a dilated duct in the head and uncinate process(c). Images of the dilated duct with stranding mucoid material and a mass in the distal duct are noted on the ERCP. Mucus was seen emanating from the papilla at ERCP. A diagnosis of mucinous duct ectasia (IPMT) was made. A papillary mucus secreting adenoma was found at surgery consistent with the clinical diagnosis. 40378c Courtesy Ashley Davidoff MD
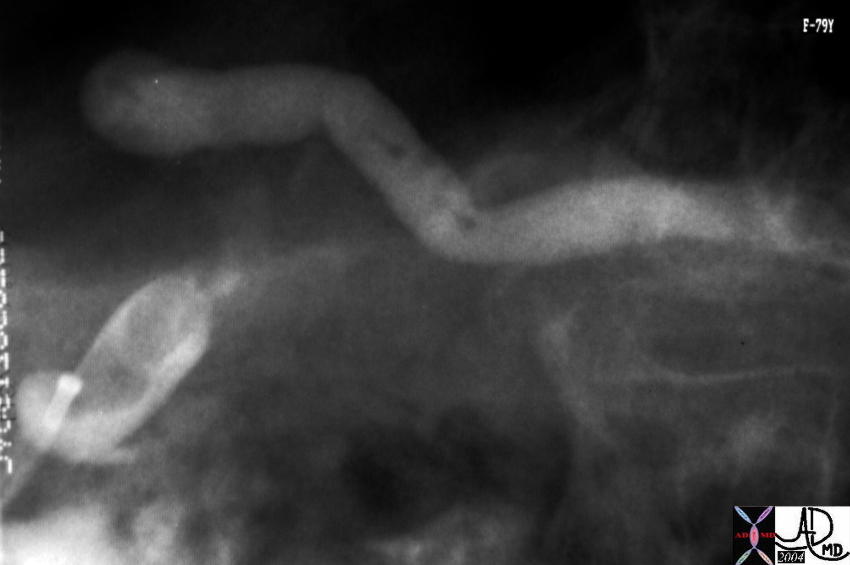 This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
References
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, Sunamura M, Furukawa T, Yanagisawa A, Ariyama J, Takada T, Watanabe H, Suda K: Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor.
Pancreas 2004, 28(3):241-246. [PubMed Abstract][Publisher Full Text]
Thompson LD, Becker RC, Przygodzki RM, Adair CF, Heffess CS: Mucinous cystic neoplasm (mucinous cystadenocarcinoma of low-grade malignant potential) of the pancreas: a clinicopathologic study of 130 cases.
Am J Surg Pathol 1999, 23(1):1-16. [PubMed Abstract][Publisher Full Text]
Wilentz RE, Albores-Saavedra J, Hruban RH: Mucinous cystic neoplasms of the pancreas.
Semin Diagn Pathol 2000, 17(1):31-42. [PubMed Abstract]
Zamboni G, Scarpa A, Bogina G, Iacono C, Bassi C, Talamini G, Sessa F, Capella C, Solcia E, Rickaert F, Mariuzzi GM, Kloppel G: Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors.
Am J Surg Pathol 1999, 23(4):410-422. [PubMed Abstract][Publisher Full Text]
Kloppel G, Luttges J: WHO-classification 2000: exocrine pancreatic tumors.
Verh Dtsch Ges Pathol 2001, 85:219-228. [PubMed Abstract]
van den Berg W, Tascilar M, Offerhaus GJ, Albores-Saavedra J, Wenig BM, Hruban RH, Gabrielson E: Pancreatic mucinous cystic neoplasms with sarcomatous stroma: molecular evidence for monoclonal origin with subsequent divergence of the epithelial and sarcomatous components.
Mod Pathol 2000, 13(1):86-91. [PubMed Abstract][Publisher Full Text]
Web references
Khan AN MD e Medicine |
 This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity in the head of the pancreas. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla. The findings are consistent with the diagnosis of IPMT.18143 Courtesy Ashley Davidoff MD
This CTscan through the head of the pancreas shows a small complex and heterogeneous mass, with dominant hypodensity in the head of the pancreas. The anatomic differential diagnosis lies between the duct and the parenchyma. An ERCP was performed showing extensive mucus production coming through the ampulla. The findings are consistent with the diagnosis of IPMT.18143 Courtesy Ashley Davidoff MD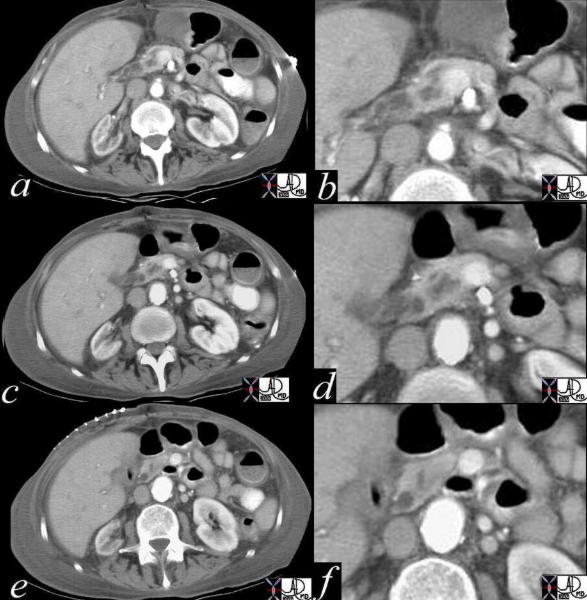 This series of images are from a CT scan of the abdomen taken through the head of the pancreas. Images a,c,and e are magnified in b,d,and f. A heterogeneous and enlarged duct is (a,b,c,d) while the downstream normal appearing duct is seen just before it joins with the bile duct. (e,f) . 18144c01 Courtesy Ashley Davidoff MD
This series of images are from a CT scan of the abdomen taken through the head of the pancreas. Images a,c,and e are magnified in b,d,and f. A heterogeneous and enlarged duct is (a,b,c,d) while the downstream normal appearing duct is seen just before it joins with the bile duct. (e,f) . 18144c01 Courtesy Ashley Davidoff MD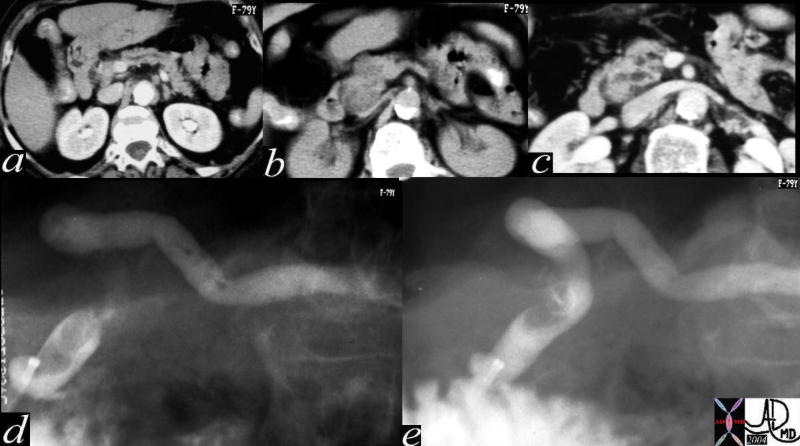 This first series of images are from a CT scan of the abdomen taken through the body and head of the pancreas. A minimally dilated pancreatic duct is noted in the body and neck (a), a heterogeneous mass in the head (b), and a dilated duct in the head and uncinate process(c). Images of the dilated duct with stranding mucoid material and a mass in the distal duct are noted on the ERCP. Mucus was seen emanating from the papilla at ERCP. A diagnosis of mucinous duct ectasia (IPMT) was made. A papillary mucus secreting adenoma was found at surgery consistent with the clinical diagnosis. 40378c Courtesy Ashley Davidoff MD
This first series of images are from a CT scan of the abdomen taken through the body and head of the pancreas. A minimally dilated pancreatic duct is noted in the body and neck (a), a heterogeneous mass in the head (b), and a dilated duct in the head and uncinate process(c). Images of the dilated duct with stranding mucoid material and a mass in the distal duct are noted on the ERCP. Mucus was seen emanating from the papilla at ERCP. A diagnosis of mucinous duct ectasia (IPMT) was made. A papillary mucus secreting adenoma was found at surgery consistent with the clinical diagnosis. 40378c Courtesy Ashley Davidoff MD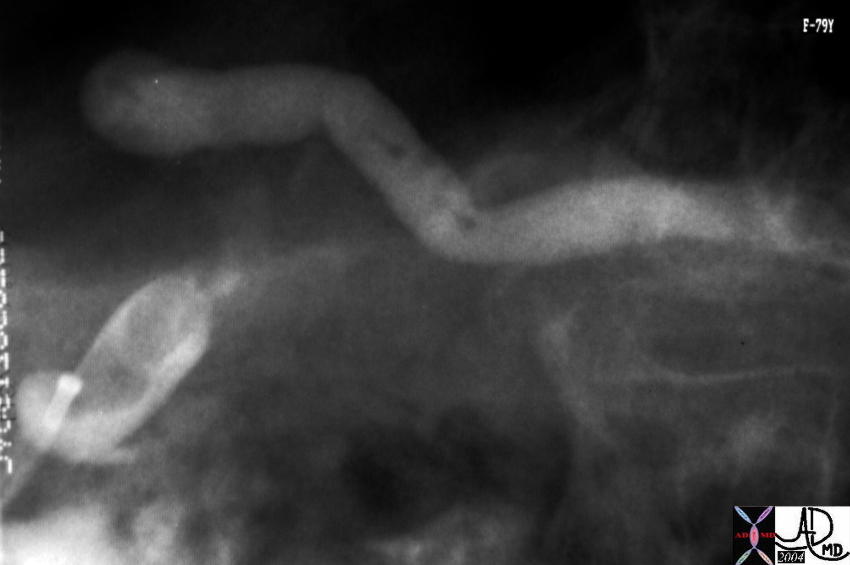 This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD
This ERCP image shows a contrast filled and dilated pancreatic duct. At ERCP mucoid material was noted in the ampulla. The lesion identified in the uncinate process on the CT was noted as a nodule in the duct. Associated findings included tubular thin and stranding filling defects in the duct of the body consistent with mucus. A diagnosis of mucinous duct ectasia with a papillary tumor with papillary and mucinous features was made at pathology. A papillary adenoma was found at surgery. 40377 Courtesy Ashley Davidoff MD